For parents and their new baby, feeding can be a time when great relationships are formed; however, it can also be a great source of anxiety and concern for parents of premature babies. Having a baby born not as expected, whether sick or premature, can be life-changing but know that you are not alone. Also know, that there is support available to help you cope and navigate the NICU and life at home. Along with connecting with others going through a similar experience, visit: www.miraclebabies.org.au to find relevant information and resources.
In the womb, your baby received all of its nutrients via the placenta and umbilical cord. When your baby is delivered premature or sick, he or she will need to receive these vital nutrients in a variety of different ways. Breast milk is important for all babies but it provides vital health benefits for premature and sick newborns and acts as a medicine that only a mother can provide.
Research has shown that the composition of a mother’s breast milk is different if her baby is born premature than if her baby was born full-term. It is tailored to the needs of a premature gut and is highly beneficial for your baby.
This milk is higher in nitrogen, protein, lipids, fatty acids, vitamins, calcium and other vital elements important to the development of premmies. Although it can be exhausting and challenging, most mothers find that providing breast milk for their baby is one of the more beneficial and rewarding things they can do.
At first, the milk you express is called colostrum. You will only produce minimal amounts, but it is extremely concentrated and rich in nutrients and antibodies. Due to the thick, sometimes sticky consistency, you may find it easier to hand express and use a syringe to collect as much colostrum as you can. Once your mature milk comes in, you will need to express frequently (eight to ten times a day) to establish and maintain your milk supply. After a few weeks or months, when you’ve established your supply, you may be able to reduce the number of times you express. Expressing breast milk is a skill that takes time to learn, and in the first few days after giving birth, you may only collect drops of milk. Please don’t get discouraged; remember that each drop is like a medicine for your baby, and it is helping get them off to a healthier start.
The requirements for collecting breast milk for sick or premature infants in hospital are more stringent than for healthy babies at home. Midwives, lactation consultants, early childhood nurses and Australian Breastfeeding Association counsellors are available to provide advice about expressing, both in hospital and at home.
There are three methods of expressing: hand expressing, hand pump expressing, and electric pump expressing. Your choice will depend on your reason for expressing and your personal preference. The hand expressing method has many advantages; it’s convenient, and the skin-to-skin contact stimulates milk production. However, hand pump expressing or electric pump expressing may be preferable for longer-term use. The following general hints apply, regardless of the method you choose:
- Express in a comfortable, private place
- Put your phone on silent, or even in another room if it’s distracting
- Have a glass of water nearby
- Have all expressing equipment within arms reach
- Help your body relax. Try listening to music, reading and book or watching tv.
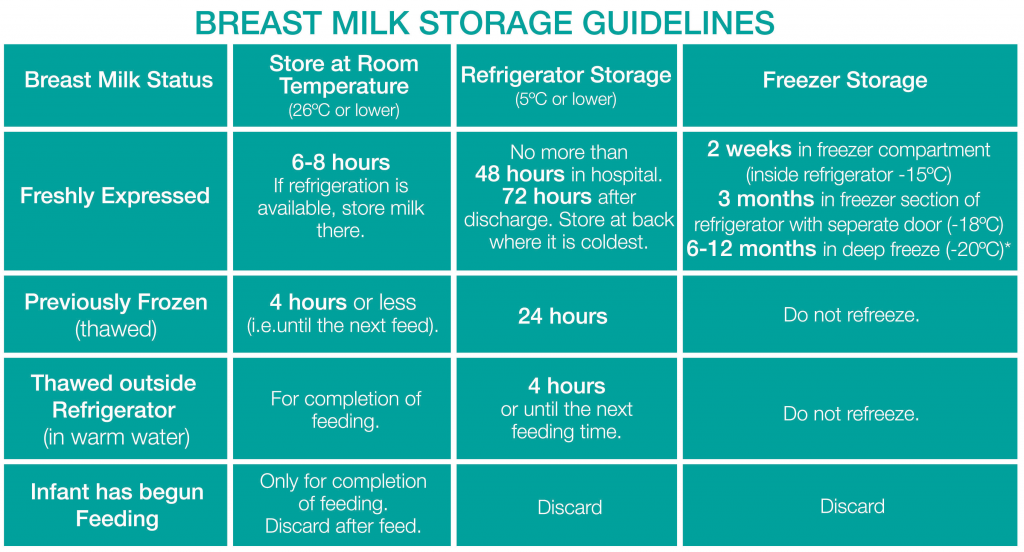
Guide to storing expressed breast milk at home:
- Wash hands thoroughly with soap and water – hands must be thoroughly dried with a clean towel, single-use towel or hand dryer
- Refrigerate or freeze milk after expressing
- Use fresh milk whenever possible
- Freeze milk that will not be used within two days
- Date the container at the time of collection and use the oldest milk first
- Transport breast milk in an insulated container – an esky with a freezer brick
- If milk has thawed, it should be used within 4 hours
In some instances, NICU babies will be given donor milk during their hospital stay. It is an important part of your baby’s care and treatment plan and will only be used as an alternative. The World Health Organisation recommends that donated breast milk is a better alternative to infant formula when the mothers’ milk is not available. This can be an excellent alternative when your baby is in the NICU or SCN. Some hospitals have their own donor milk bank, whilst others have their donor milk supplied by the Australian Red Cross LifeBlood Milk Bank.
